Blog
Digital mental health programs are inexpensive and creative. But are they working?
Almost half of Australians will experience Mental health problems in life. Recent floods, drought, cyclones, bush and pandemia because Increased suffering in the community.
However, many people in need of mental health services are Cannot be obtained. The costs, stigma and availability of mental health workers are Barriers in care. Australia also has a critical shortage of mental health workers. And until 2030, This is expected We will lack 42% of the mental labor force needed to satisfy demand.
To partially solve this gap, the Australian government involved Investing $ 135 million in digital mental health programs if it is selected.
Online mental health programs can be more creative and cheaper than other types of therapy. But do they actually work? Let’s assess the evidence.
What are digital mental health services?
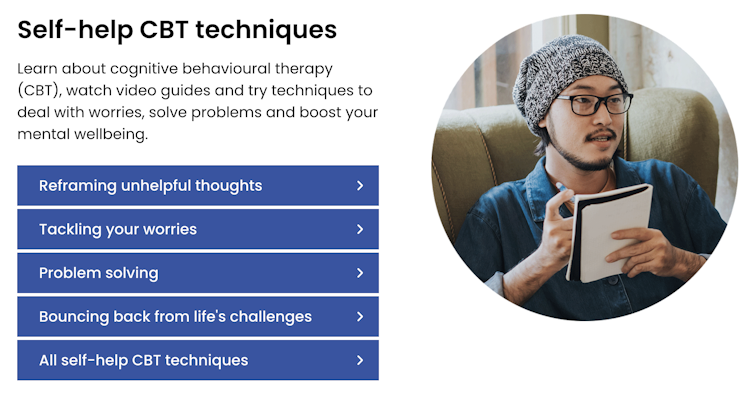
Digital mental health services differ significantly. They include information on online mental health or application, tools for tracking symptoms and learning or skill programs. These tools can be obtained with or without the support of a therapist or trainer, and some operate generative artificial intelligence (AI) and machine learning.
The umbrella term “Digital Mental Health Services” also includes peer networks, telephone helpline and teeth services on the phone, chat or teiling -based screening.
Services such as Mindspot,
Mindspot (screenshot)
Digital mental health services are targeted by a number of mental health problems, such as depression, anxiety, trauma and eating disorders. Some are intended for specific groups of people, including culturally diverse communities, LGBTQia+people, modern parents and juvenile people.
With so many digital options available, finding the right program can be arduous. Financed by the government Medicare Mental Health Portal He was created to aid Australians find services based on evidence.
Medicare Mental Health (Screenshot)
Are they working?
Review of the evidence found at 2020 Almost half This was used by people who used online programs for joint mental health conditions.
This review included Online programs with self -threading lessons or modules to reduce the symptoms of depression or anxiety. These programs were just as effective as face to face, but face -to -face therapy required an average of 7.8 times more therapist’s time than online programs.
Evidence of other types of digital mental health programs is still developing.
For example, evidence of application for smartphones focused on mental health symptoms is mixed. One sec Some Studies have shown the benefits of mental health from using such applications, others did not report differences in symptoms. Researchers suggest These applications should be used with other mental health brackets, not as independent interventions.
Similarly, while the AI chatbots received A recent attentionThere is uncertainty about the safety and effectiveness of these tools as a substitute for therapy.
Chatbots such as AI “Waebot“In the case of depression, it can provide users with personalized tips and support to learn therapeutic techniques. But although chatbots can potentially improve mental health, the results are largely inconclusive Until now. Is also no regulation in this field.
Early research show Some benefits from digital approaches in the treatment of more elaborate mental health conditions, such as suicidal and psychosis. But further research is needed.
Do users like them?
Users have reported many benefits to digital mental health services. People Find them comfortable, available, private and inexpensive and are often Very happy with them.
Digital services have been designed to directly deal with some of the main barriers in access to treatment and can reach a significant number of people who go to the Internet to obtain information about mental health.
Digital services can also be used in the “care” approach to treating mental health problems. This means that people with less elaborate or less weighty symptoms first try a low -intensity digital program before “accelerating” to more intensive support. National Health Service of Great Britain Conversation therapy program Uses this model.
NHS/Each mind matters (screenshot)
But some people still prefer face -to -face services. Grounds This includes internet communication problems, the perceived lack of treatment and personal connection, as well as concerns about the quality of care.
Some Australians face challenges related to digital skills and Internet access, which hinders to engage in online services.
Privacy concerns may also discourage people from using digital platforms, because they are worried about how their personal data is stored and made available.
What do clinicians think about them?
Mental health specialists increased their use Digital mental health tools (such as Consultations of Sweekly) clearly during Covid pandemic. However, many clinicians try to operate these tools because they have not received sufficient training or support.
Even when they are willing, clinicians face barriers in the workplace that hinder their inclusion in their practice. These include:
- Restricted financing and reimbursement of costs
- unclear rules related to liability and risk management, data storage and security
- Disturbances of work flow, such as the integration of these tools with existing systems, customer training to operate them and monitor their operate.

VH-Studio/Shutterstock
Some clinicians stay skeptic About whether digital services can really match the quality of personal therapy, which leads to hesitation in the recommendation of them to people who can operate.
What must happen next?
With mental illness and suicide estimated at the expense Australian economy $ 70 billion a year, there are forceful personal, social and financial reasons for supporting creative solutions that boost access to mental health services.
But in order for digital approaches to achieving full potential, we must boost the power of work in the field of mental health and support organizations to include digital technologies for their practice.
It is also crucial to improve the consciousness of digital mental health programs and reduce barriers to access to these services or we Risk left The people who need them the most.
In the case of Australians with more elaborate mental health problems or those for whom digital mental health treatment did not work, access to personal therapy and other mental health should remain available. Digital mental health programs are part of the psychiatric care system, and all types of care are replaced.
If you or someone you know, need aid or support, you can call Lifeline at 13 11 14.

