Blog
Taking antivirals for Covid too often depends on where you live and how wealthy you are
Medical experts recommend antiviral drugs for people aged 70 and over who contract Covid, as well as for other groups at risk of severe disease and hospitalization due to Covid.
However, many older Australians have missed out on antiviral medications after contracting Covid-19. This is yet another way the healthcare system fails the most vulnerable.
Who missed?
We analyzed COVID-related antiviral utilize from March 2022 to September 2023 We found that some groups were at higher risk of missing antivirals, including indigenous peoples, people from disadvantaged areas and people from culturally diverse backgrounds and linguistically.
Some of the differences will be due to different infection rates. However, during these 18 months, many older Australians were infected at least once, and infection rates were higher in some disadvantaged communities.
How clear are the differences?
Compared to the national average, Indigenous Australians were almost 25% less likely to be exposed to antivirals, older people living in disadvantaged areas were 20% less likely to be ill, and people from a culturally or linguistically diverse background were 13% less likely to get the disease for antiviral drugs. scenario.
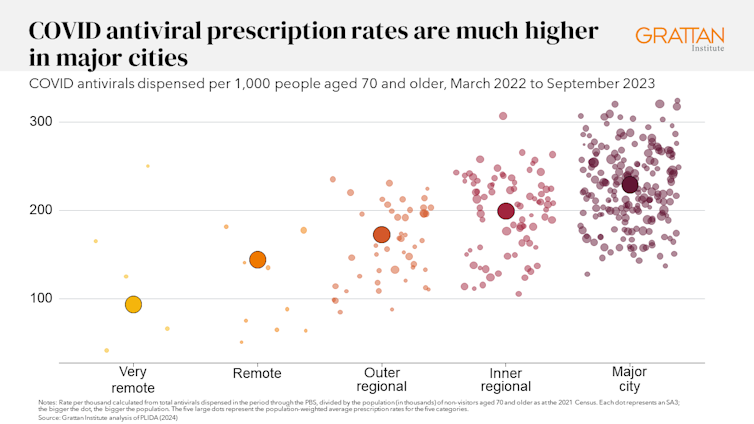
People living in remote areas were 37% less likely to become infected with antivirals than those living in vast cities. People from outer regional areas were 25% less likely to do so.
Grattan Institute
Even within the same city, the differences are clear. In Sydney, people over the age of 70 from the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were almost twice as likely to be taking antiviral drugs than those in Fairfield in Sydney’s southwest.
Older people in Melbourne’s leafy inner east (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to be taking the antiviral drug than those in Brimbank (including Sunshine) in the city’s west.
Grattan Institute
Why do people miss?
Antiviral drugs for Covid should be taken as soon as the first symptoms appear. Although awareness about antiviral drugs for Covid is generally high, people often don’t realize they would benefit from the medicine. They Wait until the symptoms worsen and it is too tardy.
Recurrent visits to your family doctor make a massive difference. Our analysis found that people aged 70 and over, who were more likely to visit their GP, were significantly more likely to receive antiviral drugs for Covid.
Regular visits provide an opportunity for prevention and patient education. For example, GPs can provide high-risk patients with ‘COVID treatment plans’ as a reminder to get tested and seek treatment as soon as they feel unwell.
Difficulty seeing a GP may support explain the low uptake of antiviral drugs in rural areas. Compared to residents of vast cities, residents of compact rural towns have approximately 35% less GPs visit their GP half as often and are 30% more likely to be seen report waiting too long for an appointment.
Just like for Vaccineprimary care physicians’ focus on antiviral medications likely makes a difference, as does ensuring care is accessible to people from diverse cultural backgrounds.
Care should belong to those who need it
Since the period we analyzed, evidence has emerged that raises doubts doubts about the effectiveness of antiviral drugs, especially in people at lower risk of severe disease. This means that vaccination is more crucial than taking antiviral drugs.
However, all Australians eligible for antivirals should have the same chance of getting them.
These drugs cost more than A$1.7 billion, with the extensive majority of that money coming from the federal government. Although spending rates have dropped, over 30,000 In August, packages of antiviral drugs for Covid were released, costing about $35 million.
Such a huge investment should not leave so many people behind. Getting treatment should not depend on your income, cultural background or place of residence. Instead, care should be targeted at those who need it most.

National Cancer Institute/Unsplash
People born abroad were 40% more likely die from Covid-19 than those born here. Indigenous Australians were 60% more likely die from Covid-19 than non-Indigenous people. And these were people in the most disadvantaged situations 2.8 times are more likely to die from Covid-19 than residents of the richest areas.
Antivirals were more likely to be omitted for all risk groups.
This isn’t just a problem with antivirals. These same groups also disproportionately lose access to information about Covid-19 Vaccineincreasing the risk of severe disease. The pattern repeats with other crucial preventive health care measures such as cancer film adaptation.
A three-step plan to meet patient needs
The federal government should do three things to fill these gaps in preventive care.
First, the government should make primary health networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with primary care physicians and step in to boost service utilization in communities that lack primary care.
Secondly, the government should extend it My Medicare reforms. MyMedicare provides general practices with versatile financing for the care of patients who live in aged care homes or frequently visit hospital. This should be the approach expanded all patients, while providing more resources for poorer and sicker patients. This will give GP practices time to inform patients about preventive health care, including Covid vaccines and antiviral drugs, before they become ill.
Thirdly, team prescribing by pharmacists should be introduced. Pharmacists could then quickly dispense antiviral drugs to patients if they had previously agreed this with the patient’s GP. This approach would also work for drugs for chronic diseases such as cardiovascular disease.
Antiviral drugs for Covid, unlike vaccines, keep up with novel variants without requiring updates. If a novel, more harmful variant of the disease emerges, or if a novel pandemic hits, governments should implement these systems to ensure that everyone who needs treatment receives it quickly.
In the meantime, more equitable access to care will support close massive and lasting closures gaps health between different groups of Australians.

